In the high-stakes world of modern medicine, data is the new lifeblood. From electronic health records (EHRs) to real-time genomic sequencing, healthcare providers are sitting on a goldmine of information. However, for decades, the “pickaxe” required to extract value from this data, Healthcare Data Analysis with No-Code AI, was locked behind a wall of complex code and prohibitively expensive development teams.
The landscape is shifting. The democratization of AI, driven by the rise of No-Code AI platforms, is putting the power of data science directly into the hands of clinicians, researchers, and hospital administrators. This isn’t just a technical upgrade; it’s a fundamental shift in how we save lives and manage resources through Healthcare Data Analysis with No-Code AI.
Launch Your App Today
Ready to launch? Skip the tech stress. Describe, Build, Launch in three simple steps.
BuildThe Dawn of No-Code AI in the Medical Sector
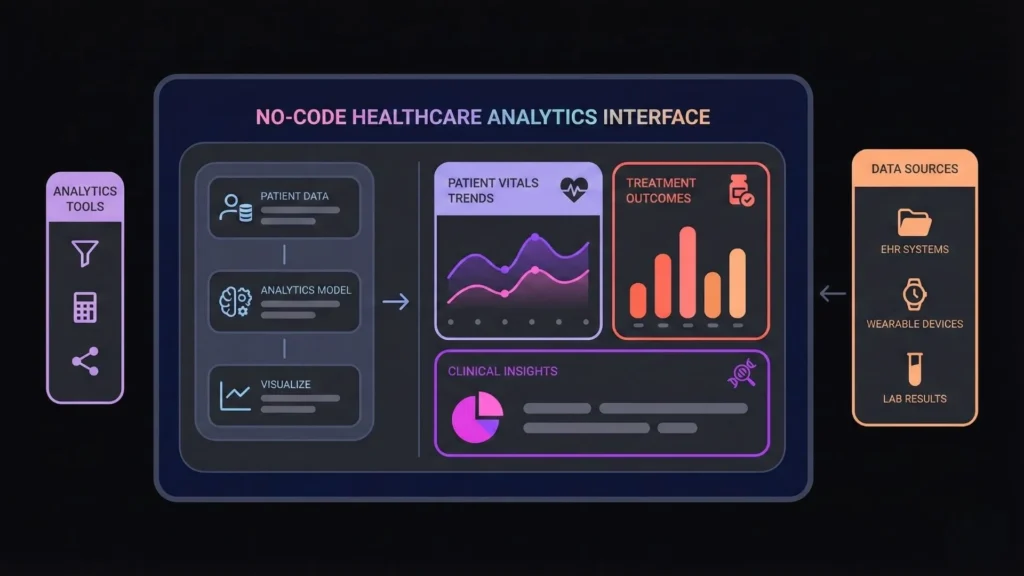
Historically, if a hospital wanted to build a predictive model to identify patients at risk of sepsis, they needed a team of data scientists and months of custom software development. Today, user-friendly, drag-and-drop interfaces allow a nurse manager or a specialized researcher to build and deploy those same models in a fraction of the time, leveraging the power of Healthcare Data Analysis with No-Code AI.
The Impact of Accessibility
By removing the “coding barrier,” we are seeing a surge in localized innovation across the medical landscape. Smaller clinics that were previously priced out of the AI revolution can now participate in high-level research. In fact, medical studies utilizing no-code methodologies have seen a 30% increase since 2020. This inclusivity is fostering a collaborative environment where the people closest to the patients—the clinicians—are the ones designing the tools, enhancing the field of Healthcare Data Analysis with No-Code AI.
Bridging the Engineering Gap with Imagine.bo
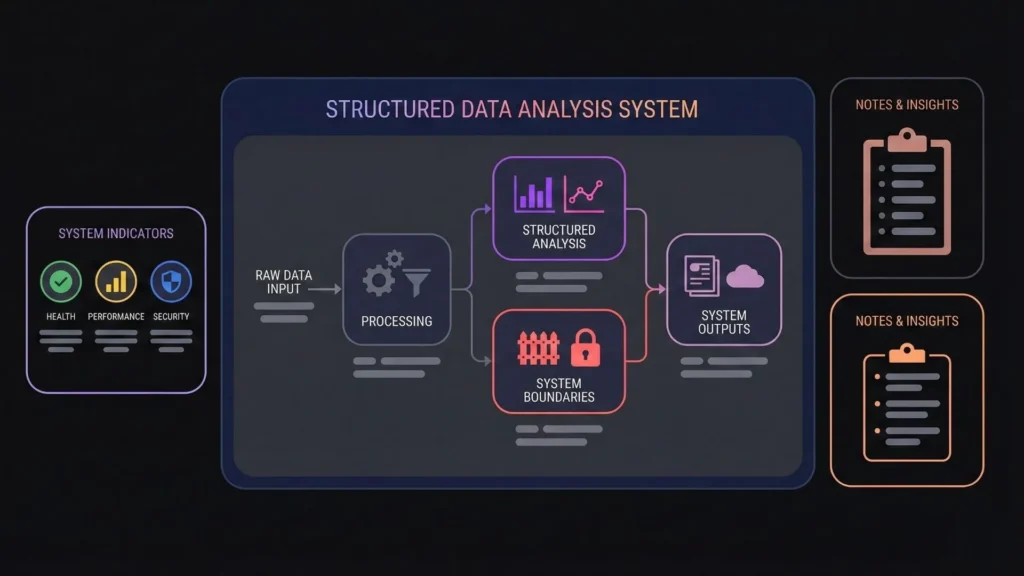
While accessibility is great, healthcare requires a level of precision that “simple” no-code tools often lack. This is where professional-grade builders like Imagine.bo come into play. Instead of just creating a basic dashboard, Imagine.bo utilizes an AI Reasoning Engine to build “SDE-level” (Software Development Engineer) applications. It ensures that the clinical tools you build today are scalable, secure, and production-ready from day one, not just prototypes, all under the umbrella of Healthcare Data Analysis with No-Code AI.
Why No-Code is the Perfect Match for Healthcare Data
Healthcare data is messy. It’s vast, unstructured (like physician notes), and strictly regulated by laws like HIPAA and GDPR. Traditional coding methods often struggle to keep up with the rapid pace of clinical needs.
Speed as a Lifesaver
In a fast-moving healthcare environment, time is the most critical variable. A project that would take a traditional dev team six months to code can often be tackled in weeks or even days using a no-code platform. Whether it’s identifying an emerging public health threat or optimizing a vaccine rollout, the speed of no-code allows for a “proactive” rather than “reactive” stance.
The Intuitive Advantage
Most healthcare professionals are not programmers, nor should they have to be. No-code platforms offer intuitive interfaces that minimize the learning curve. This empowers:
- Clinicians: To analyze patient trends to optimize treatment protocols.
- Administrators: To leverage predictive models for better resource allocation.
- Researchers: To quickly test hypotheses against massive datasets without waiting for IT approval.
Navigating the Benefits and Limitations
As with any transformative technology, it is essential to balance the “hype” with the “reality.”
The Core Benefits
- Reduced Development Costs: Building custom AI apps manually can cost hundreds of thousands of dollars. No-code platforms like Imagine.bo save tens of thousands by automating the backend, frontend, and QA.
- Clinical Relevance: When clinicians build the tool, the tool solves clinical problems. There is no “lost in translation” moment between a doctor and a developer.
- Rapid Iteration: Healthcare guidelines change. No-code allows you to update your logic instantly without rewriting thousands of lines of code.
The Limitations (and How to Solve Them)
A common pitfall is the “Black Box” nature of some AI. Doctors need to know why a model made a specific prediction. Furthermore, generic no-code tools might struggle with niche data, like oncology-specific imaging.
The Solution: Choose a platform that prioritizes Model Explainability. Modern AI builders now provide visual insights into feature importance, helping medical professionals trust the results. Moreover, using a platform like Imagine.bo ensures that the underlying architecture is “clean code,” making it easier to audit and refine than a closed-source “black box” system.
Choosing the Right No-Code AI Tool: A Buyer’s Guide
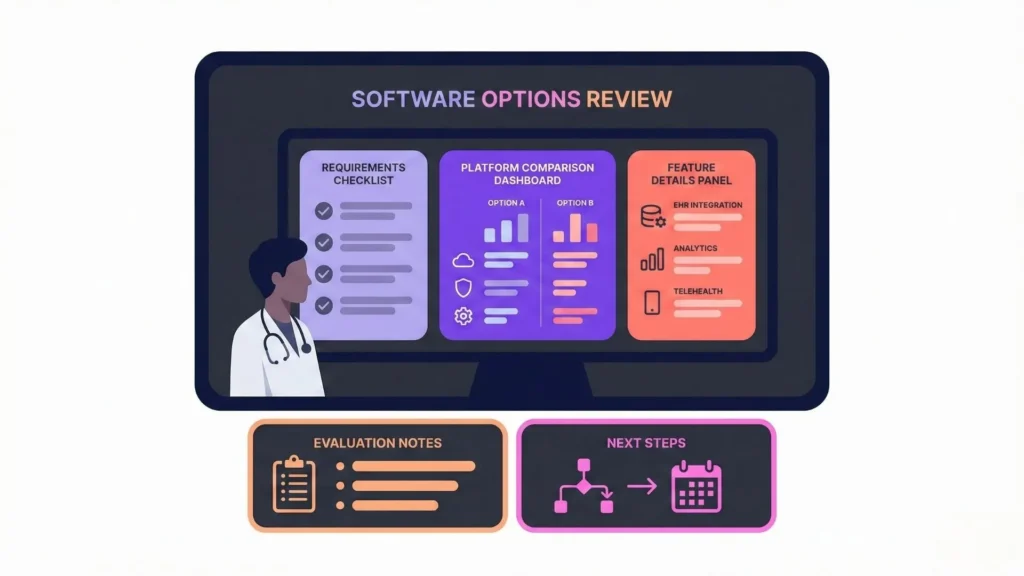
Not all no-code tools are created equal, especially for the medical field. When evaluating a platform, focus on these three pillars:
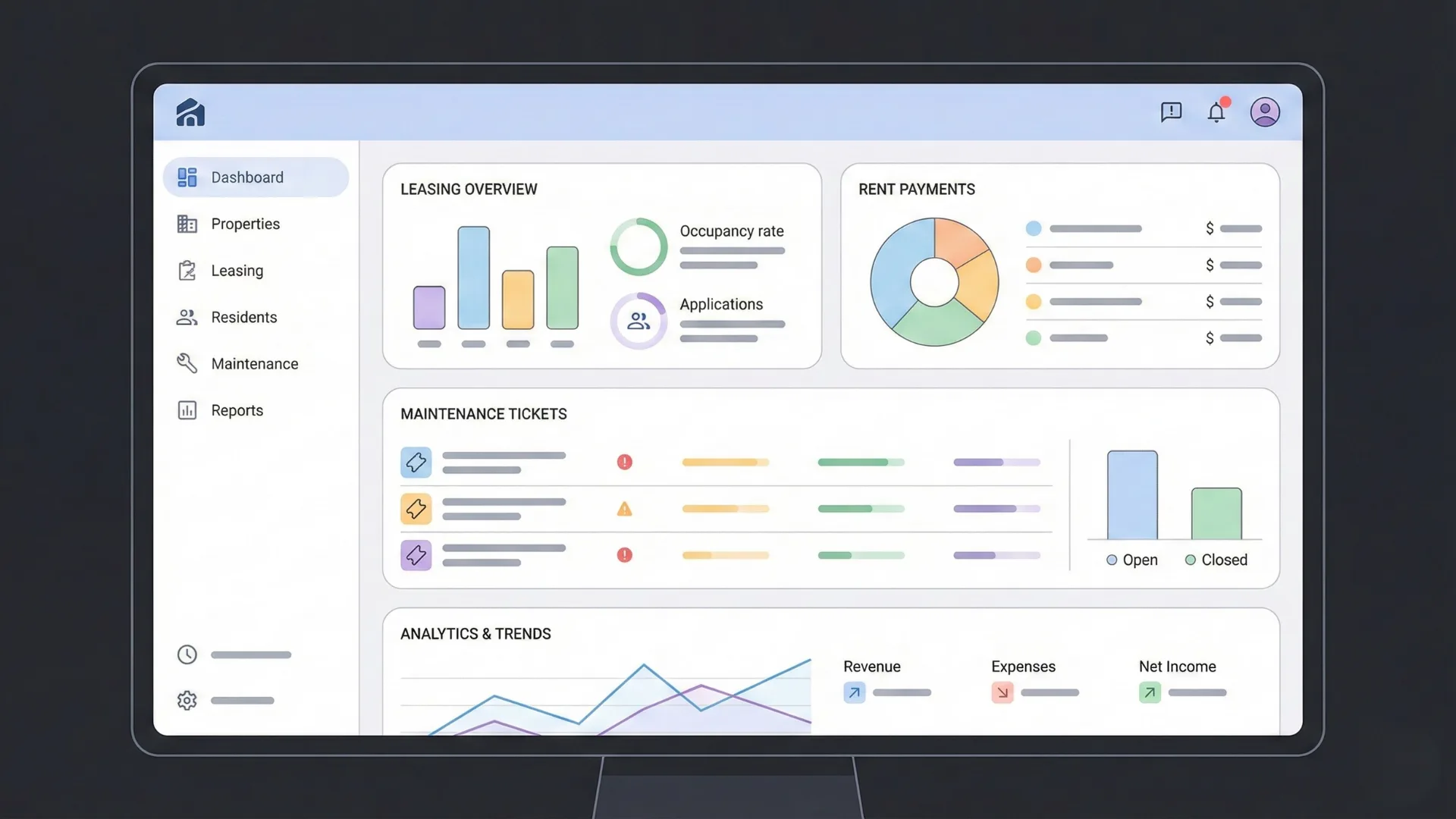
I. Healthcare-Specific Functionality
Look for platforms that offer pre-built connectors for EHR systems. A tool that understands the structure of lab results or physician notes will save you hundreds of hours in data cleaning.
II. Enterprise-Grade Security
In healthcare, security isn’t a feature; it’s a prerequisite. Ensure your chosen platform is GDPR and SOC2-ready to protect sensitive patient information. Additional requirements include:
- Equipped with data encryption both in transit and at rest.
- Capable of handling high-performance execution (e.g., Imagine.bo supports up to 1,000 transactions per second, making it ideal for large-scale hospital operations).
III. SDE-Level Architecture
Most no-code builders create “spaghetti code” in the background that breaks as soon as you scale. For a medical app, you need an AI No-Code App Builder that follows real engineering standards. Imagine.bo excels here by generating scalable backend logic and secure data handling that mirrors the work of a senior software engineer.
Practical Applications: From Theory to the Operating Room

How is this actually being used today? Let’s look at three high-impact areas.
A. Improved Diagnostics and Treatment
By combining structured data (vitals) with unstructured data (clinical notes) through Natural Language Processing (NLP), clinicians are seeing a 15-20% boost in diagnostic accuracy.
- Example: Using AI to analyze heart failure risk factors hidden in EHRs allows for earlier intervention, significantly reducing readmission rates.
B. Predictive Modeling for Resource Allocation
Hospitals use predictive models to forecast bed demand and staffing needs. By analyzing historical flow and even local weather patterns, administrators can preemptively allocate resources to handle surges. This minimizes disruptions and ensures that a patient never waits longer than necessary for a critical care bed.
C. Optimizing Operational Efficiency
Inefficiency in the Operating Room (OR) is a major cost driver. No-code AI can analyze surgeon preferences, equipment sterilization cycles, and procedure durations to create an “optimal” schedule. One study showed that just a 10% reduction in appointment time through AI-driven optimization led to a 5% increase in patient throughput.
How Imagine.bo Redefines the Healthcare App Journey
If you are a founder or a healthcare leader with a vision, you don’t just need a “data tool” you need a way to turn that data into a functional, revenue-ready product. Imagine.bo provides a unique 5-step workflow designed to move from vision to launch seamlessly:
- Vision Definition: Describe your healthcare problem in plain English.
- AI Reasoning: The engine maps out user flows and recommends a tech stack (AWS, GCP, or Vercel).
- Seamless Development: It generates the frontend, backend, and databases with automated QA.
- Confident Launch: One-click deployment into a secure, HIPAA-compliant environment.
- Human + AI Support: Continuous updates and the ability to assign custom tasks to professional developers for hyper-specialized logic.
Step-by-Step: Performing Your Own Data Analysis
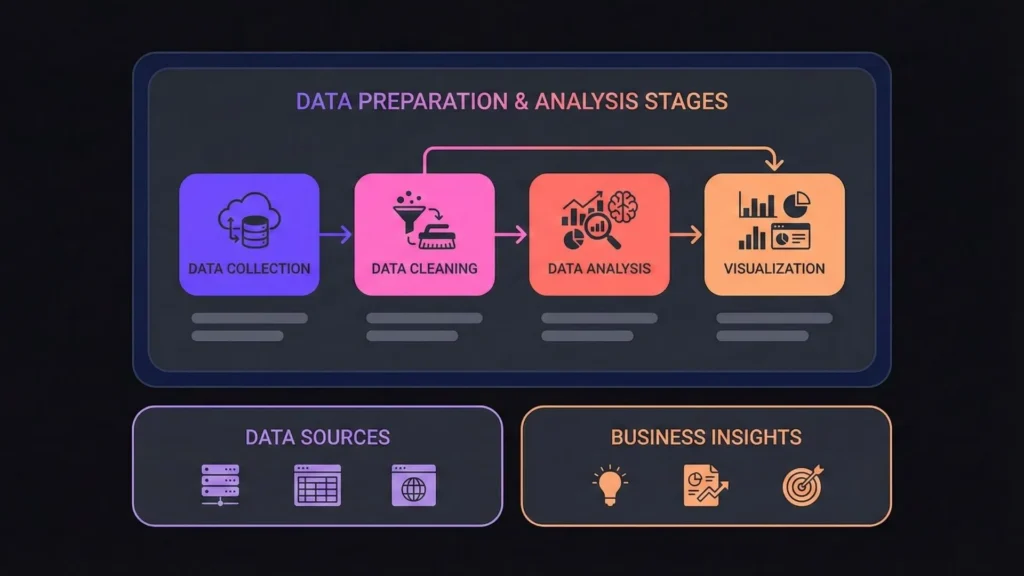
If you’re ready to start, follow this clinical framework for successful analysis:
Step 1: Data Preparation (The 80% Rule)
Data cleaning is the most important stage.
- Address Missing Values: Use imputation techniques to fill gaps in patient records.
- Handle Outliers: Identify if an extreme value is a data entry error or a unique clinical case.
- Feature Selection: Use Principal Component Analysis (PCA) to find the variables that actually matter.
Step 2: Training the Model
Choose your algorithm based on your goal. Use Classification for disease prediction and Regression for cost or time estimations. Always split your data into “Training” and “Validation” sets to ensure your model works on “new” patients.
Step 3: Interpreting and Actioning Insights
Interpreting and actioning insights from a no-code AI analysis requires clinical context. Don’t just look at the numbers; look at the Confidence Intervals. A 70% risk of readmission with a wide margin of error is a signal for more testing, not an immediate clinical decision. Use visualizations like heatmaps to communicate these risks.
Ethical Challenges and the Path Forward
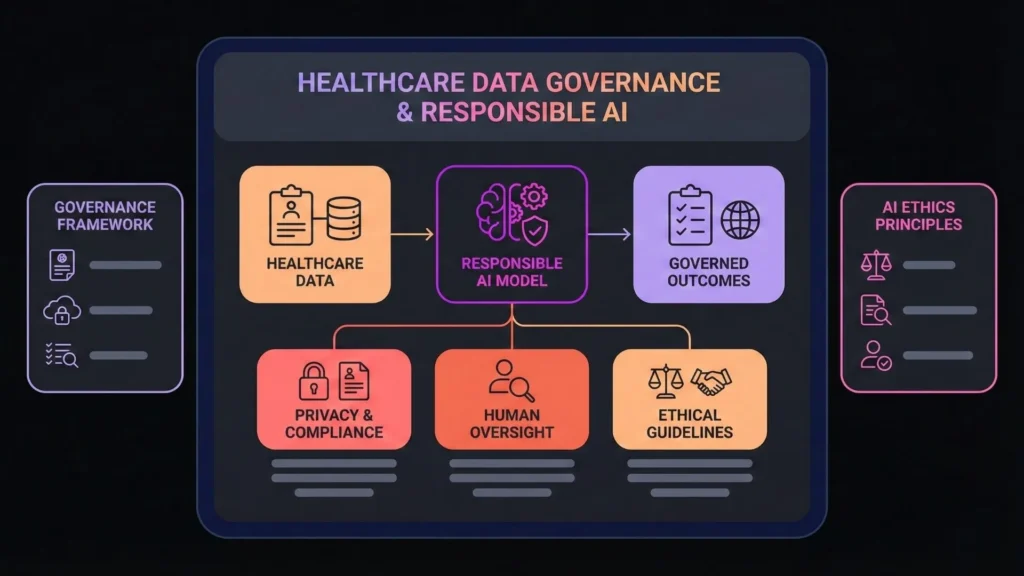
The “AI Doctor” isn’t here to replace the “Human Doctor.” It’s here to augment them.
Ethical Challenges
Addressing ethical challenges is vital as AI grows in healthcare. AI is only as fair as the data it’s trained on. If your dataset lacks diversity, your AI might misdiagnose underrepresented groups. Successful healthcare AI requires Human Oversight and regular audits to ensure equity.
Data Privacy
Maintaining strict data privacy and compliance standards is mandatory. Sophisticated techniques like Federated Learning are becoming the standard. This allows multiple hospitals to train a shared AI model without ever actually sharing or moving sensitive patient data, keeping privacy intact while maximizing intelligence.
The Role of Human Oversight
We envision a future where clinicians leverage tools like Imagine.bo to build their own custom dashboards and diagnostic aids. However, the final clinical judgment will always rest with the human professional. AI provides the “what” and the “how,” but the “why” remains a human endeavor.
Conclusion: The Future of Your Healthcare Vision
The transition from data-rich to insight-rich is no longer a luxury it’s a necessity. With platforms like Imagine.bo, the barriers to entry have vanished, allowing you to build the future of healthcare vision you’ve always imagined. You can now describe a complex medical problem in plain English and watch as AI builds a secure, SDE-level application to solve it.
Whether you are an entrepreneur looking to disrupt the diagnostic space or a hospital leader aiming to optimize your OR, the tools are ready. It’s time to unlock the insights hidden in your data and build the future of healthcare, one no-code app at a time.
Ready to turn your healthcare vision into a production-grade app? Explore Imagine.bo and start building today.
SEO Metadata (Internal Use)
- Focus Keyword: No-Code AI Healthcare Data Analysis
- Secondary Keywords: Healthcare App Builder, AI Medical Insights, Predictive Modeling Healthcare, Imagine.bo, HIPAA Compliant AI.
- Meta Description: Discover how no-code AI is revolutionizing healthcare data analysis. Learn how to build SDE-level medical apps with Imagine.bo without writing a single line of code.
Launch Your App Today
Ready to launch? Skip the tech stress. Describe, Build, Launch in three simple steps.
Build